The World Well being Group has recommended a new name for monkeypox, asking international locations to neglect the unique time period in favor of a brand new one, “mpox,” that scientists hope will assist destigmatize the illness. However in america, the request appears to be arriving late. The outbreak right here has been in gradual retreat for months—and has already left many Individuals’ minds.
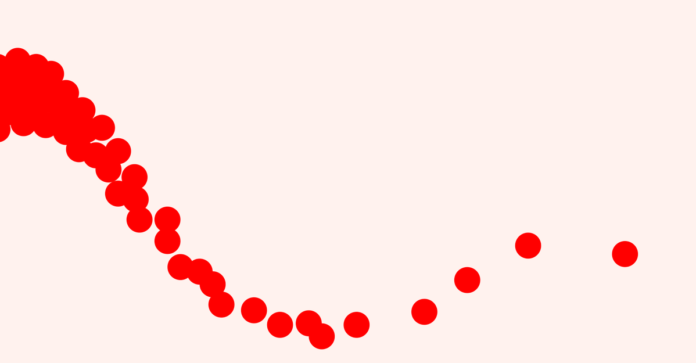
About 15 instances at the moment are being recorded amongst Individuals every day, lower than 4 p.c of the tally when the surge was at its worst. After a sluggish and bungled early rollout, checks and coverings for the virus are extra obtainable; more than a million doses of the two-shot Jynneos smallpox vaccine have discovered their method into arms. San Francisco and New York—two of the nation’s first cities to declare mpox a public-health emergency this previous summer season—have since allowed those orders to expire; so have the states of New York and Illinois. “I believe that is the endgame,” says Caitlin Rivers, an infectious-disease epidemiologist on the Johns Hopkins Heart for Well being Safety.
However “endgame” doesn’t imply “over”—and mpox will likely be with us for the foreseeable future. The U.S. outbreak is just now exhibiting us its lengthy and ugly tail: 15 day by day instances just isn’t zero day by day instances; even because the variety of new infections declines, inequities are growing. Black and Latino folks make up a majority of new mpox cases and are contracting the illness at three to five times the speed of white Individuals, however they’ve acquired proportionately fewer vaccines. “Now it’s really the oldsters who’re essentially the most marginalized that we’re seeing,” says Ofole Mgbako, a doctor and population-health researcher at New York College. “Which can also be why, in fact, it’s fallen out of the information.” If the virus sticks round (because it very seemingly might), and if the disparities persist (as they virtually definitely will), then mpox might find yourself saddling hundreds of weak Individuals annually with one more debilitating, stigmatized, and uncared for illness.
At this level, there’s not even any assure that this case downturn will persist. “I’m not satisfied that we’re out of the woods,” says Sara Bares, an infectious-disease doctor on the College of Nebraska Medical Heart, in Omaha. Immunity, acquired by an infection or vaccines, is now concentrated amongst these at highest threat, says Jay Varma, a doctor and epidemiologist at Weill Cornell Medication. However researchers nonetheless don’t know how well these defenses can stave off one other an infection, or how lengthy they may final—gaps in data that could be robust to fill, now that incidence is so low. And though months of advocacy and outreach from the LGBTQ group have cut down risky sexual activities, many cautionary tendencies will finally reset to their pre-outbreak norm. “We all know extensively from different sexually transmissible infections that conduct change just isn’t often essentially the most sustained response,” says Boghuma Kabisen Titanji, an infectious-disease doctor at Emory College.
On the identical time, this yr’s mpox outbreaks are stranger and extra unwieldy than people who got here earlier than. A ballooning physique of proof suggests that folks can turn out to be infectious before they develop symptoms, opposite to prior understanding; some physicians are involved that sufferers, particularly those that are immunocompromised, would possibly stay infectious after the brunt of visible illness resolves, says Philip Ponce, an infectious-disease doctor on the College of Texas Well being Science Heart at San Antonio and the medical director of San Antonio’s Variety Clinic. (Some 40 percent of Individuals who’ve been recognized with mpox live with HIV.) Researchers nonetheless don’t have a great grip on which bodily fluids and types of contact could also be riskiest over the trajectory of a illness. Instances are nonetheless being missed by primary-care suppliers who stay unfamiliar with the ins and outs of analysis and testing, particularly in folks with darker pores and skin. And though this epidemic has, for essentially the most half, continued to have an effect on males who’ve intercourse with males, women and nonbinary people are getting sick as properly, to an underappreciated diploma.
Intel on the one mpox-fighting antiviral on the shelf, a smallpox drug referred to as tecovirimat, additionally stays concerningly scant, at the same time as consultants fear that the virus might develop resistance. The therapy has been given a conditional green light to be used in people who find themselves presently, or liable to turning into, severely sick. Anecdotally, it appears to work wonders, shaving days or perhaps weeks off the painful, debilitating course of signs that may ship contaminated folks into long-term isolation. However consultants nonetheless lack rigorous information in people to verify simply how properly it really works, Bares, who’s among the many scientists concerned in a nationwide study of the antiviral, instructed me. And though clinical trials for tecovirimat are under way, she added, within the U.S., they’re “struggling to enroll sufferers” now that infections have plummeted to such a sustained low. It’s a numerical drawback in addition to a sociocultural one. “The urgency with which individuals reply questions declines as case counts go down,” Varma instructed me.
Recent CDC reports present {that a} rising proportion of latest infections aren’t being reported with a recognized sexual-contact historical past, stymieing efforts at contact tracing. Which may partly be a product of the outbreak’s gradual migration from liberal, well-off city facilities, hit early on within the epidemic, to extra communities in the South and Southwest. “In small cities, the chance of disclosure is excessive,” Bares instructed me. In in search of care or vaccination, “you’re outing your self.” When mpox instances in Nebraska took an surprising nosedive earlier this fall, “a colleague and I requested each other, ‘Do you suppose sufferers are afraid to return in?’” These issues will be particularly excessive in sure communities of coloration, Ponce instructed me. San Antonio’s Latino inhabitants, as an illustration, “tends to be rather more conservative; there’s rather more stigma related to one being LGBT in any respect, not to mention being LGBT and attempting to entry biomedical interventions.”
Hidden infections can turn out to be fast-spreading ones. Monitoring an infectious illness is way simpler when the folks most in danger have insurance coverage protection and entry to savvy clinicians, and when they’re inclined to belief public-health establishments. “That’s predominantly white folks,” says Ace Robinson, the CEO of the Pierce County AIDS Basis, in Washington. Now that the mpox outbreak is transferring out of that inhabitants into much less privileged ones, Robinson fears “a large undercount” of instances.
Individuals who’re catching the virus in the course of the outbreak’s denouement are paying a value. The means to combat mpox are prone to dwindle, even because the virus entrenches itself within the inhabitants most in want of these instruments. One concern stays the country’s vaccination strategy, which underwent a mid-outbreak shift: To handle restricted shot provide, the FDA licensed a brand new dosing technique with restricted proof behind it—a call that primarily affected folks close to the again of the inoculation line. The strategy is secure however tough to manage, and it may have robust negative effects: A few of Titanji’s sufferers have skilled swelling close to their injection website that lasted for weeks after their first dose, and now “they simply don’t need to get one other shot.”
The continued shift of mpox into minority populations, Robinson instructed me, can also be additional sapping public consideration: “So long as that is centered in BIPOC communities, there’s going to be much less of a push.” Public curiosity on this disaster was modest even at its highest level, says Steven Klemow, an infectious-disease doctor at Methodist Dallas Medical Heart and the medical director of Dallas’s Variety Clinic. Now consultants are watching that cycle of neglect reinforce itself because the outbreak continues to have an effect on and compress into marginalized communities, together with people who have for many years borne a disproportionate share of the burden of sexually related infections reminiscent of syphilis, gonorrhea, and HIV. “These will not be the teams that essentially get folks leaping on their toes,” Titanji instructed me.
Among the folks most in danger are transferring on as properly, Robinson instructed me. In his group in Washington, he was disillusioned to see excessive charges of vaccine refusal at two latest outreach occasions serving the area’s Black and American Indian populations. “That they had no data of the virus,” he instructed me. Titanji has seen related tendencies in her group in Georgia. “There’s some sense of complacency, like, ‘It’s not a difficulty, so why do I have to get vaccinated?’” she mentioned.
The tide appears unlikely to shift. Even tens of hundreds of instances deep into the American outbreak, sexual-health clinics—which have been on the entrance strains of the mpox response—stay quick on funds and workers. Though the inflow of instances has slowed, Ponce and Klemow are nonetheless treating a number of mpox sufferers every week whereas attempting to maintain up the companies they sometimes supply—at a time when STI rates are on a years-long rise. “We’re actually assuming that that is going to turn out to be one other sexually related illness that’s going to be part of our wheelhouse that we’ll need to handle for the indefinite future,” Klemow instructed me. “We’ve needed to pull assets away from our different companies that we offer.” The issue might but worsen if the national emergency declared in August is allowed to run out, which might seemingly curb the availability of antivirals and vaccines.
Rivers nonetheless holds out hope for eliminating mpox within the U.S. However getting from low to zero isn’t as straightforward because it might sound. This present stretch of decline might unspool for years, even many years, particularly if the virus finds a new animal host. “We’ve seen this story play out so many instances earlier than,” Varma instructed me. Efforts to remove syphilis from the U.S. in the late ’90s and early 2000s, as an illustration, gained traction for some time—then petered out throughout what might have been their last stretch. It’s the basic boom-bust cycle to which the nation is so susceptible: As case charges fall, so does curiosity in pushing them additional down.
Our recollections of public-health crises by no means appear to linger for lengthy. In the beginning of this mpox outbreak, Titanji instructed me, there was a possibility to shore up our programs and buffer ourselves in opposition to future epidemics, each imported and homegrown. The nation squandered it and did not ship help overseas. If one other surge of mpox instances arrives, because it very seemingly might, she mentioned, “we are going to once more be going again to the drafting board.”