Again within the spring, across the finish of the COVID-19 public-health emergency, hospitals across the nation underwent a change in gown code. The masks that employees had been sporting at work for greater than three years vanished, in some locations in a single day. At UChicago Medication, the place masking insurance policies softened on the finish of Could, Emily Landon, the manager medical director of an infection prevention and management, fielded hate mail from colleagues, some chiding her for ready too lengthy to carry the requirement, others accusing her of imperiling the immunocompromised. At Vanderbilt College Medical Heart, which did away with masking in April, forward of many establishments, Tom Talbot, the chief hospital epidemiologist, was inundated with thank-yous. “Individuals had been prepared; they had been drained,” he informed me. “They’d been asking for a number of months earlier than that, ‘Can we not cease?’”
However throughout hospitals and insurance policies, infection-prevention specialists shared one sentiment: They felt virtually sure that the masks would wish to return, doubtless by the top of the calendar yr. The large query was precisely when.
For some hospitals, the reply is now. In latest weeks, as COVID-19 hospitalizations have been rising nationwide, stricter masking necessities have returned to a smattering of hospitals in Massachusetts, California, and New York. However what’s taking place across the nation is hardly uniform. The approaching respiratory-virus season would be the nation’s first after the end of the public-health emergency—its first, because the arrival of COVID, with out crisis-caliber funding put aside, routine monitoring of neighborhood unfold, and health-care precautions already in place. After years of preventing COVID in live performance, hospitals are again to going it alone.
A return to masking has a transparent logic in hospitals. Sick sufferers come into shut contact; medical procedures produce aerosols. “It’s an ideal storm for potential transmission of microbes,” Costi David Sifri, the director of hospital epidemiology at UVA Well being, informed me. Hospitals are on the entrance traces of illness response: They, greater than practically another place, should prioritize defending society’s susceptible. And with yet one more lethal respiratory virus now in winter’s repertoire, precautions ought to logically enhance in lockstep. However “there is no such thing as a clear reply on how to do that proper,” says Cameron Wolfe, an infectious-disease doctor at Duke. Individuals have already staked out their stances on masks, and now hospitals should function inside these confines.
When hospitals moved away from masking this spring, they every did so at their very own tempo—and settled on very completely different baselines. Like many different hospitals in Massachusetts, Brigham and Girls’s Hospital dropped its masks mandate on Could 12, the day the public-health emergency expired; “it was a noticeable distinction, simply strolling across the hospital” that day, Meghan Baker, a hospital epidemiologist for each Brigham and Girls’s Hospital and Dana-Farber Most cancers Institute, informed me. UVA Well being, in the meantime, weaned employees off of common masking over the course of about 10 weeks.
Most masks on the Brigham at the moment are donned on solely a case-by-case foundation: when a affected person has lively respiratory signs, say, or when a health-care employee has been not too long ago sick or uncovered to the coronavirus. Workers additionally nonetheless masks across the identical subset of susceptible sufferers that acquired further safety earlier than the pandemic, together with bone-marrow-transplant sufferers and others who’re extremely immunocompromised, says Chanu Rhee, an affiliate hospital epidemiologist at Brigham and Girls’s Hospital. UVA Well being, in the meantime, is requiring masks for everybody within the hospital’s highest-risk areas—amongst them, sure intensive-care models, in addition to most cancers, transplant, and infusion wards. And though Brigham sufferers can at all times request that their suppliers masks, at UVA, all sufferers are requested upon admission whether or not they’d like hospital employees to masks.
Almost each professional I spoke with informed me they anticipated that masks would in some unspecified time in the future come again. However in contrast to the early days of the pandemic, “there may be mainly no steering from the highest now,” Saskia Popescu, an epidemiologist and infection-prevention professional on the College of Maryland Faculty of Medication, mentioned. The CDC nonetheless has a webpage with advice on when to mask. These suggestions are tailor-made to most people, although—and don’t advise protecting up till COVID hospital admissions go “approach excessive, when the horse has nicely and really left the barn,” Landon, at UChicago, informed me. “In well being care, we have to do one thing earlier than that”—tamping down transmission prior to wards filling up.
Extra particular recommendation might nonetheless emerge from the CDC, or particular person state well being departments. However going ahead, the idea is that “every hospital is meant to have its personal normal plan,” Rhee informed me. (I reached out to the CDC repeatedly about whether or not it’d replace its infection-prevention-guidance webpage for COVID—final retooled in Could—however didn’t obtain a response.)
Which leaves hospitals with one in every of two attainable paths. They may schedule a begin to masking season, primarily based on after they estimate instances may rise—or they might react to information as they arrive in, tying masking insurance policies to transmission bumps. With SARS-CoV-2 nonetheless so unpredictable, many hospitals are choosing the latter. That additionally means defining a real case rise—“what I feel everyone is battling proper now,” Rhee mentioned. There is no such thing as a common definition, nonetheless, for what constitutes a surge. And with extra immunity layered over the inhabitants, fewer infections are leading to extreme illness and demise—even, to a limited extent, lengthy COVID—making numbers that may have triggered mitigations only a yr or two in the past now much less pressing catalysts.
Additional clouding the forecast is the truth that a lot of the info that specialists as soon as relied on to watch COVID in the neighborhood have pale away. In most elements of the nation, COVID instances are now not recurrently tallied; persons are both not testing, or testing solely at house. Wastewater surveillance and methods that monitor all influenza-like diseases might present some help. However that’s not a complete lot to go on, particularly in elements of the nation reminiscent of Tennessee, the place sewage isn’t as closely tracked, Tom Talbot, of Vanderbilt, informed me.
Some hospitals have turned as an alternative to in-house stats. At Duke—which has adopted a mitigation coverage that’s similar to UVA’s—Wolfe has mulled pulling the more-masking lever when respiratory viruses account for two to 4 p.c of emergency and urgent-care visits; at UVA, Sifri has thought of taking motion as soon as 1 or 2 p.c of staff name out sick, with the goal of staunching illness and preserving employees. “It actually doesn’t take a lot to have an effect on our capacity to keep up operations,” Sifri informed me. However “I don’t know if these are the best numbers.” Plus, inner metrics at the moment are difficult for a similar causes they’ve gotten shaky elsewhere, says Xiaoyan Music, the chief infection-control officer at Kids’s Nationwide Hospital, in Washington, D.C. Screening is now not routine for sufferers, skewing positivity stats; even sniffly health-care staff, a number of specialists informed me, at the moment are much less keen to check and report.
For hospitals which have maintained a extra masky baseline, situations by which common masking returns are just a little simpler to ascertain and enact. At UChicago Medication, Landon and her colleagues have developed a color-coded system that begins at teal—masking for high-risk sufferers, sufferers who request masked care, and anybody with signs, plus masking in high-risk areas—and goes by everyone-mask-up-everywhere crimson; their staff plans to satisfy weekly to evaluate the state of affairs, primarily based on quite a lot of neighborhood and inner metrics, and march their masking up or down. Wolfe, of Duke, informed me that his hospital “wished to order just a little bit of additional masking fairly deliberately,” in order that any shift again towards stricter requirements would really feel like much less of a shock: Habits are laborious to interrupt after which reform.
Different hospitals which have been dwelling largely maskless for months, although, have an extended highway again to common masking, and employees members who won’t be recreation for the trek. Ought to masks have to return on the Brigham or Dana-Farber, as an example, “I believe the response might be blended,” Baker informed me. “So we actually are attempting to be even handed.” The hospital may attempt to protect some maskless zones in places of work and ready rooms, as an example, or lower-risk rooms. And at Kids’s Nationwide, which has additionally largely executed away with masks, Music plans to follow the local health department’s lead. “As soon as D.C. Well being requires hospitals to reimplement the universal-masking coverage,” she informed me, “we might be implementing it too.”
Different mitigations are on the desk. A number of hospital epidemiologists informed me they anticipated to reimplement some extent of asymptomatic screening for varied viruses across the identical time they reinstate masks. However measures reminiscent of visiting restrictions are a harder name. Wolfe is reluctant to tug that lever earlier than he completely has to: Going by a hospital keep alone is without doubt one of the “more durable issues for sufferers to endure.”
A bespoke strategy to hospital masking isn’t impractical. COVID waves received’t occur synchronously throughout communities, and so maybe neither ought to insurance policies. However hospitals that lack the assets to maintain tabs on viral unfold will doubtless be at an obstacle, and Popescu informed me she worries that “we’re going to see important transmission” within the very establishments least geared up to deal with such inflow. Even the best-resourced locations might hit hindrances: Many are nonetheless reeling from three-plus years of disaster and are coping with nursing shortages and employee burnout.
Coordination hasn’t fully gone away. In North Carolina, Duke is working with the College of North Carolina at Chapel Hill and North Carolina State College to shift insurance policies in tandem; in Washington State, a number of regional health-care organizations have pledged to align their masking insurance policies. And the Veterans Well being Administration—the place masking stays required in high-risk models—has developed a playbook for augmenting mitigations throughout its many services, which collectively make up the nation’s largest built-in health-care system, says Shereef Elnahal, the undersecretary of Veterans Affairs for well being. Nonetheless, establishments can wrestle to maneuver in sync: Attitudes on masking aren’t exactly universal across health-care providers, even inside a hospital.
The nation’s expertise with COVID has made hospitals that rather more attuned to the impacts of infectious illness. Earlier than the pandemic started, Talbot mentioned, masking was a rarity in his hospital, even round high-risk sufferers; many staff would go on shifts sick. “We had been fairly complacent about influenza,” he informed me. “Individuals might come to work and unfold it.” Now hospital staff maintain themselves to a stricter normal. On the identical time, they’ve develop into intimately attuned to the drawbacks of fixed masking: Some have complained that masks intervene with communication, particularly for sufferers who’re younger or laborious of listening to, or who’ve a language barrier. “I do assume you lose just a little little bit of that non-public bonding,” Talbot mentioned. And previous to the lifting of common masking at Vanderbilt, he mentioned, some employees had been telling him that one out of 10 occasions they’d ask a affected person or household to masks, the trade would “get antagonistic.”
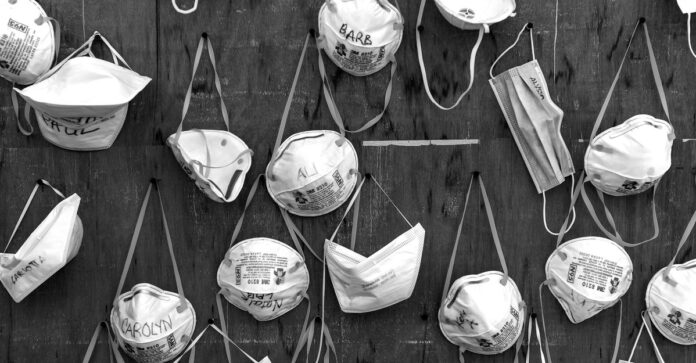
When lifting mandates, lots of the hospital epidemiologists I spoke with had been cautious to message to colleagues that the state of affairs was fluid: “We’re suspending common masking briefly,” as Landon put it to her colleagues. Nonetheless, she admits that she felt uncomfortable returning to a low-mask norm in any respect. (When she informally polled practically two dozen different hospital epidemiologists across the nation within the spring, most of them informed her that they felt the identical.) Well being-care settings aren’t meant to appear like the remainder of the world; they’re locations the place precautions are anticipated to go above and past. COVID’s arrival had cemented masks’ capacity to cease respiratory unfold in shut quarters; eradicating them felt to Landon like pushing these information apart, and placing the onus on sufferers—significantly these already much less prone to advocate for themselves—to account for their very own safety.
She will be able to nonetheless think about a United States by which a pandemic-era response solidified, because it has in a number of different international locations, right into a peacetime norm: the place sporting masks would have remained as routine as donning gloves whereas drawing blood, a tangible image of pandemic classes realized. As a substitute, many American hospitals might be getting into their fourth COVID winter trying lots like they did in early 2020—when the virus stunned us, when our defenses had been down.