“I used to be a lot much less confident now that I used to be a affected person myself,” says neurosurgeon Henry Marsh. “I abruptly felt a lot much less sure about how I might been [as a doctor], how I might dealt with sufferers, how I might spoken to them.”
Picture Supply/Getty Photographs
disguise caption
toggle caption
Picture Supply/Getty Photographs

“I used to be a lot much less confident now that I used to be a affected person myself,” says neurosurgeon Henry Marsh. “I abruptly felt a lot much less sure about how I might been [as a doctor], how I might dealt with sufferers, how I might spoken to them.”
Picture Supply/Getty Photographs
Famend British doctor Henry Marsh was one of many first neurosurgeons in England to carry out sure mind surgical procedures utilizing solely native anesthesia. For over 30 years, he additionally made frequent journeys to Ukraine, the place he carried out surgical procedure and labored to reform and replace the medical system.
As a surgeon, Marsh felt a sure degree of detachment in hospitals — till he was identified with superior prostate most cancers at age 70. Although he continued working after his prognosis, it was sobering to work together with the hospital as each a health care provider and a affected person.
“I used to be a lot much less confident now that I used to be a affected person myself,” he says. “I abruptly felt a lot much less sure about how I might been [as a doctor], how I might dealt with sufferers, how I might spoken to them.”
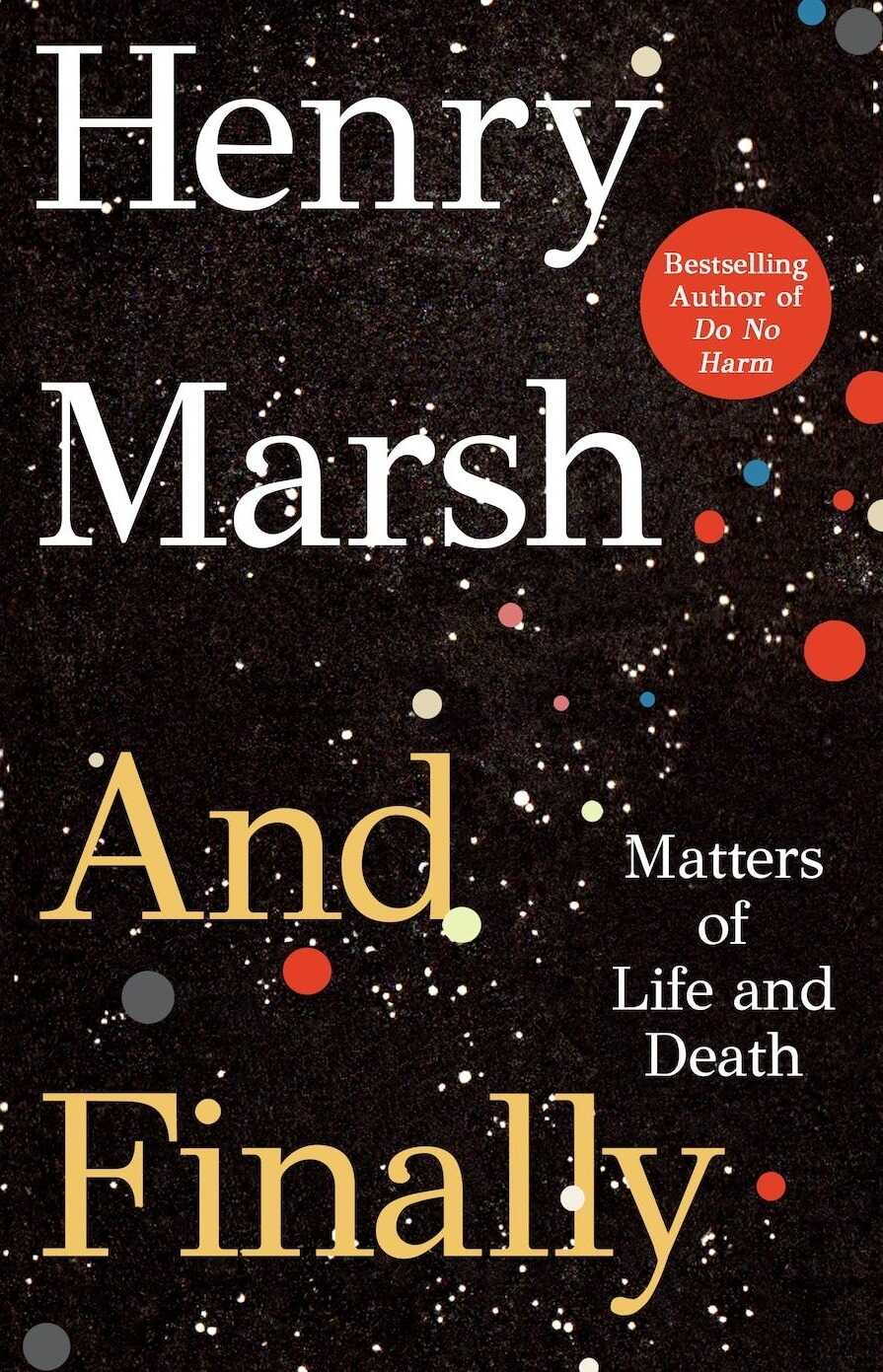
Within the memoir, And Lastly, Marsh opens up about his experiences as a most cancers affected person — and displays on why his prognosis occurred at such a sophisticated stage.
“I believe many docs reside on this kind of limbo of ‘us and them,’ ” he says. “Sickness occurs to sufferers, to not docs. Anecdotally, I am instructed that many docs current with their cancers very late, as I did. … I denied my signs for months, if not for years.”
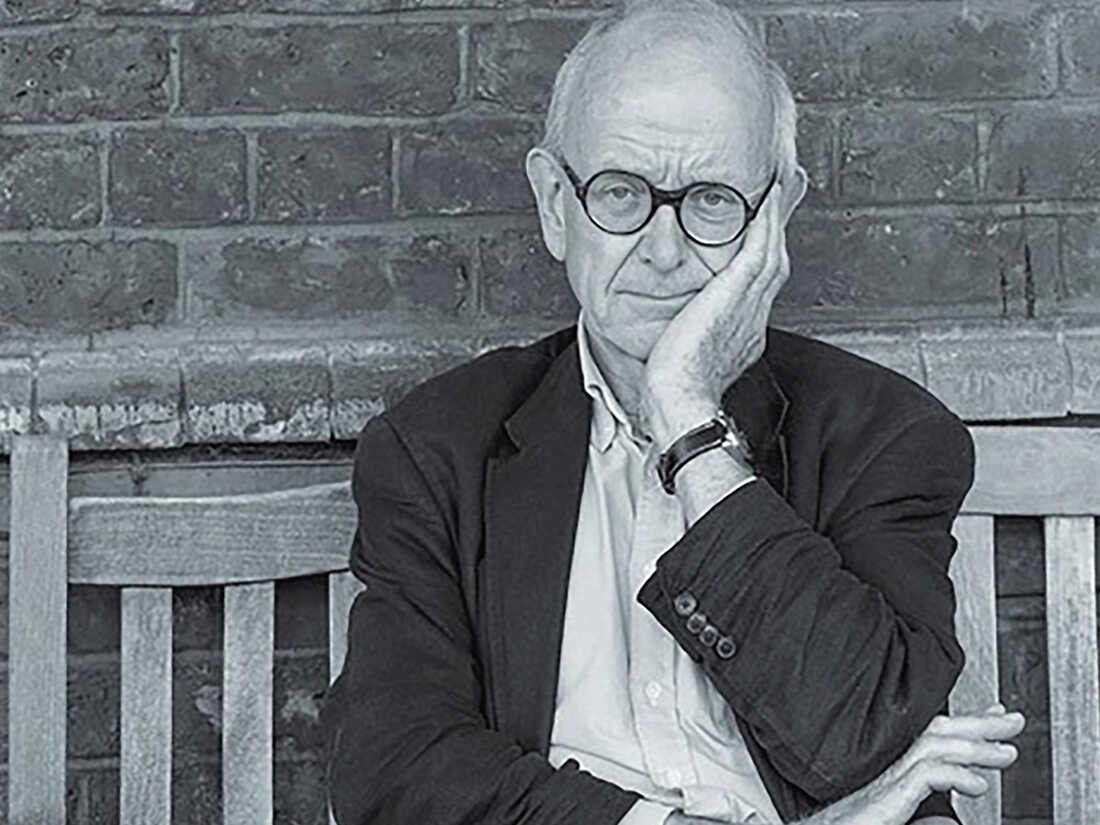
Henry Marsh was the topic of the Emmy Award-winning 2007 documentary The English Surgeon, which adopted his work in Ukraine.
Thomas Dunne Books
disguise caption
toggle caption
Thomas Dunne Books
Henry Marsh was the topic of the Emmy Award-winning 2007 documentary The English Surgeon, which adopted his work in Ukraine.
Thomas Dunne Books
Marsh’s most cancers is in remission now, however there is a 75% probability that it’ll return within the subsequent 5 years. It is an uncertainty that Marsh has realized to simply accept.
“For the previous few weeks I have been on this great Buddhist Zen-like state,” he says. “In the intervening time, I am actually very, very comfortable to be alive. However that is actually solely doable as a result of I’ve had a really full life and I’ve a really shut and loving household and people are the issues that matter in life.”
Interview Highlights
On seeing his personal mind scan, and being shocked at its indicators of age
It was the start of my having to simply accept I used to be getting previous, settle for I used to be turning into extra like a affected person than a health care provider, that I wasn’t resistant to the decay and growing old and diseases I have been seeing in my sufferers for the earlier 40 years. So it was really terribly scary wanting on the scan, crossing a threshold, and I’ve by no means dared to have a look at it once more. It was simply too upsetting. On reflection, it most likely wasn’t that huge a deal. Most likely, if I had seen that scan at work, I might have mentioned, “Nicely, that is a typical 70-year-old mind scan.”
On persevering with to work within the hospital after being identified with most cancers
As a health care provider, you are not emotionally engaged in any means. You take a look at mind scans, you hear horrible, tragic tales and you are feeling nothing, actually, on the entire, you are completely indifferent. However what I discovered was once I was at some instructing conferences and they’d see scans of a person with prostate most cancers which had unfold to the backbone and was inflicting paralysis, I might really feel a chilly clutch of concern in my coronary heart. … I might by no means felt anxious going into hospitals earlier than, as a result of I used to be indifferent. I used to be a health care provider. Sickness occurs to sufferers, to not docs.
On getting identified at age 70, and feeling his life was full
All of us need to go on dwelling. The want to go on dwelling could be very, very deep. I’ve a loving household. I’ve 4 grandchildren who I dote on. I am very busy. I am nonetheless lecturing and instructing. I’ve a workshop. I am making issues on a regular basis. There are many issues I need to go on doing, so I might prefer to have a future. However I felt very strongly because the prognosis sunk in that I might actually been very fortunate. I might reached 70. I had a very thrilling life. There are a lot of issues I used to be ashamed of and regretted, however I just like the phrase “full.” Clearly, for my spouse’s sake, my household’s sake they need me to reside longer and I need to reside longer. However purely for myself, I believe how fortunate I have been and the way usually approaching the tip of your life may be troublesome if there’s a lot of unresolved issues or troublesome relationships which have not been sorted out. So in that sense, I am able to die. Clearly, I do not need to, not but, however I am form of reconciled to it.
On not fearing demise, however fearing the struggling earlier than demise
I hate hospitals, at all times have. They’re horrible locations, although I spent most of my life working in them. It is probably not demise itself [I fear].
I do know, as a health care provider, that dying may be very disagreeable. I am a fiercely impartial particular person. I do not like being uncontrolled. I do not like being dependent upon different individuals. I cannot like being disabled and withering away with terminal sickness. I’d settle for it, I do not know. You by no means know till it occurs to you. And I do know from each household and mates and sufferers, it is wonderful what one can come to simply accept when your earlier self would throw up his or her arms in horror. So I do not know. However I would really like the choice of assisted dying if my finish seems to be like it will be slightly disagreeable.
On why he helps medically assisted demise
Medical legislation in England [is that it] is homicide to assist any individual kill themselves. It is ridiculous, is the quick reply. Suicide shouldn’t be unlawful, so you must present some fairly good explanation why it’s unlawful to assist any individual do one thing which isn’t unlawful and which is completely authorized. And opinion polls in Britain at all times present an enormous majority, 78%, need the legislation to be modified. However there is a very impassioned, dare I say it, fanatical group — primarily palliative care docs — who’re deeply against it. And so they’ve bought the ear of members of parliament.
They argue that assisted dying will result in coercion of what they name weak individuals. You already know, previous, lonely individuals will likely be in some way bullied by grasping kin or merciless docs and nurses into asking for assist in killing themselves. However there isn’t any proof that is occurring within the many international locations the place assisted dying is feasible, as a result of you may have a lot of authorized safeguards. It isn’t suicide on request. You can also make the safeguards as sturdy as you want: It’s important to apply greater than as soon as in writing, with a delay. It’s important to be seen by impartial docs who will ensure you’re not being coerced otherwise you’re not clinically depressed. So it is solely a really small quantity of people that go for it, however it does appear to work moderately nicely with out horrible issues in international locations the place it is authorized. And there isn’t any query of the actual fact, even regardless of good palliative care — though some palliative care docs deny this — dying may be very disagreeable, each not a lot bodily because the lack of dignity and autonomy, which is the prospect that troubles me.
On figuring out when it was time to cease doing surgical procedure
I finished working full time and principally working in England once I was 65, though I labored quite a bit in Kathmandu and Nepal and likewise, after all, in Ukraine. And what I at all times felt as a matter of precept, it is best to go away too early slightly than too late. As in something in life, whether or not it is a cocktail party or your skilled life itself, it is best to go away too early slightly than too late. To be sincere, I used to be getting more and more annoyed at work. I imply, I am an important believer within the British Nationwide Well being Service, however it’s turn out to be more and more bureaucratic. And psychologically, I used to be turning into much less and fewer suited to working in a really managerial bureaucratic surroundings. I am a little bit of a maverick free cannon. Additionally, I felt it is time for the following technology to take over. And I had turn out to be moderately good on the operations I did. I did not assume I used to be getting any higher. And I had an excellent trainee who may take over from me and had really taken issues ahead, and significantly within the awake craniotomy apply, he is doing significantly better issues than I may have completed. So it felt like time to go in that regard.
What actually surprises me now could be I do not miss it in any respect. I used to be utterly hooked on working, like most surgeons. The extra harmful, the tougher the operation, the extra I wished to do it, the entire danger and pleasure factor. Some of the troublesome elements of surgical procedure is studying when to not function. However a lot to my shock, I do not miss it — and I do not fairly perceive that. However I am very glad. In a humorous kind of means, I really feel like a extra full human being now that I am not a surgeon. I not have a horrible break up in my world view between me — and the medical system and my medical colleagues, that’s — and sufferers. So I really feel a extra complete particular person.
Thea Chaloner and Joel Wolfram produced and edited the audio of this interview. Bridget Bentz, Molly Seavy-Nesper and Deborah Franklin tailored it for the online.










